Health Insurance schemes including Ayushman Bharat-Arogya Karnataka (AB-ArK) are advocated by central and state governments as system for solving the problem of Out-Of-Pocket Expenditure (OOPE), a key barrier to access to health care. All the insurance schemes involve contracts with private hospitals so that low income persons and families can have expanded access to medical care (especially specialist care) because government hospitals and services have not expanded adequately to meet population needs.
SAA-K (Sarvathrika Arogya Andolaan Karnataka) conducted a study between May-July 2024, the results which show that these much-touted health insurance schemes are a myth for providing effective, cashless care. A study conducted by Janarogya Andolana Karnataka in 2012-13 also showed similar findings. Several similar studies have shown that health insurance schemes are not supporting poor families.
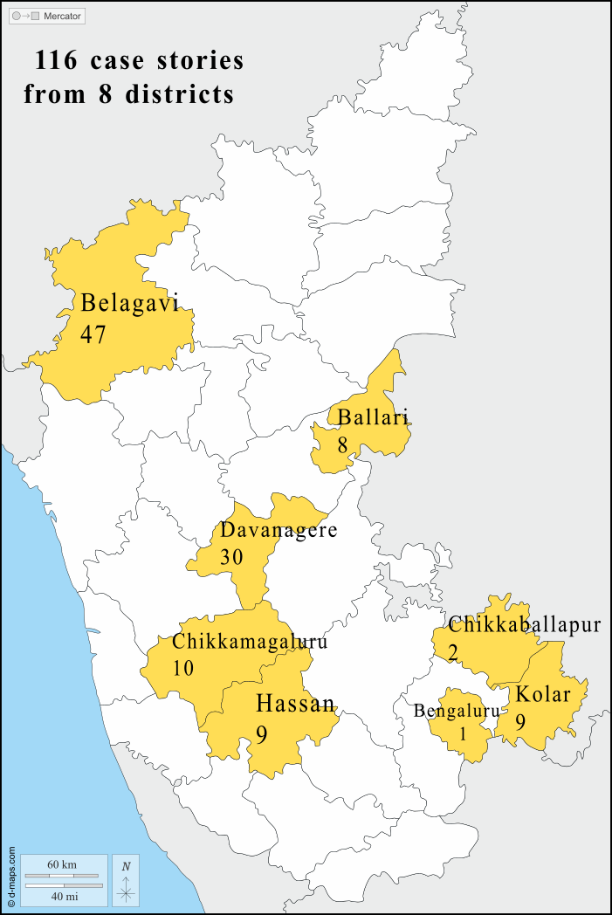
A total of 116 persons were interviewed and case stories documented from eight districts of Karnataka by SAA-K Health Activists to document the expenses and hardships incurred due to hospitalisation and to find out if State-led Health Insurance were helpful or not. Our findings presents the high OOP expenses that people are bearing for common secondary and tertiary healthcare in Karnataka and how the design and process of AB-ArK and other state-led insurance are only creating further red tape for health care and moving far from being people-centric.
Key findings:
- 102 people were admitted to government and private hospitals, and 94% of them possessed insurance.
- 17% of those admitted to government hospitals could not use their insurance, and compared to 49% admitted to private hospitals who were denied insurance coverage.
- BPL/ration cards were the most accepted form of insurance in government hospitals; in private hospitals it was AB-ArK
- Only for 5 out of 102 (4.9%) had treatment free of cost. 97/102 incurred high OOPE relative to wages.
- People on average are spending almost similar (and sometimes more) amount OOP in both government and private hospitals when they have utilised insurance as compared to when they are unable to utilise insurance.
- Insurance IS NOT reducing the OOP.
- Patients do not get to see the actual bill and the amount allocated for their treatment.
- Medicines and tests are still NOT available free of cost.
| Case story of an 8-year-old girl from Davanagere district The girl’s mother is a beedi worker and father is a daily wage construction worker. The child had difficulty walking and her neck was deviating to one side. She was taken to a private hospital 9 km away since they perceived this as an emergency, where they spent ₹36,000 on admission, MRI, tests and treatment. She was said to have a mass in her spine and that she needed to be operated. For this, she was referred to a neurosurgeon at another private hospital due to the lack of a neurosurgeon in the Government facilities. At this facility they required that the child’s name be in the ration card. Later they went to a hospital in Mangalore thinking they might treat with a parent’s ration card, spending a total of ₹10,000 on food, treatment, and other miscellaneous expenses, but there also they were asked to have daughter’s name in the ration card and to produce an AB-ArK referral letter from government facility. For 3 months, the father tried to get his daughter’s name in the ration card but the server wasn’t connecting in the state portal. They were told that it had been paused due to new enrolments for the Gruhalakshmi scheme. When the family went to the district hospital in Davanagere to get a referral letter for AB-ArK, the hospital didn’t have the “referral code” required for the diagnosis. None of the hospitals that they visited had noted this code in her documents. The family had to visit a private neurosurgeon and request him to write the referral code. He wrote this down for them with the promise that they would get treatment from their private hospital. However, without a ration card, further AB-ArK referral letters couldn’t be processed and the child remained without treatment despite spending a total of ₹46,000 spent in the process. Moreover, the father continued to lose several days of daily wages in this paperwork while the child remained ill. |
The above case story represents just one among many working-class families who are left to navigate the confusing and unaccountable pathway to care during serious sickness to get healthcare even when they possess BPL cards and insurance cards.
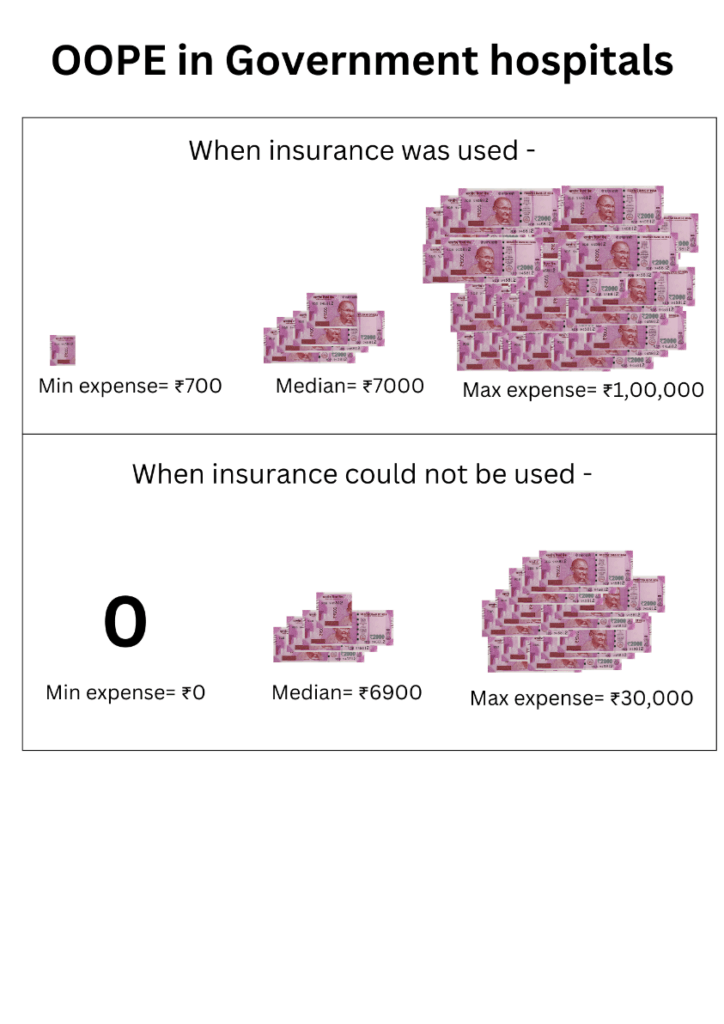
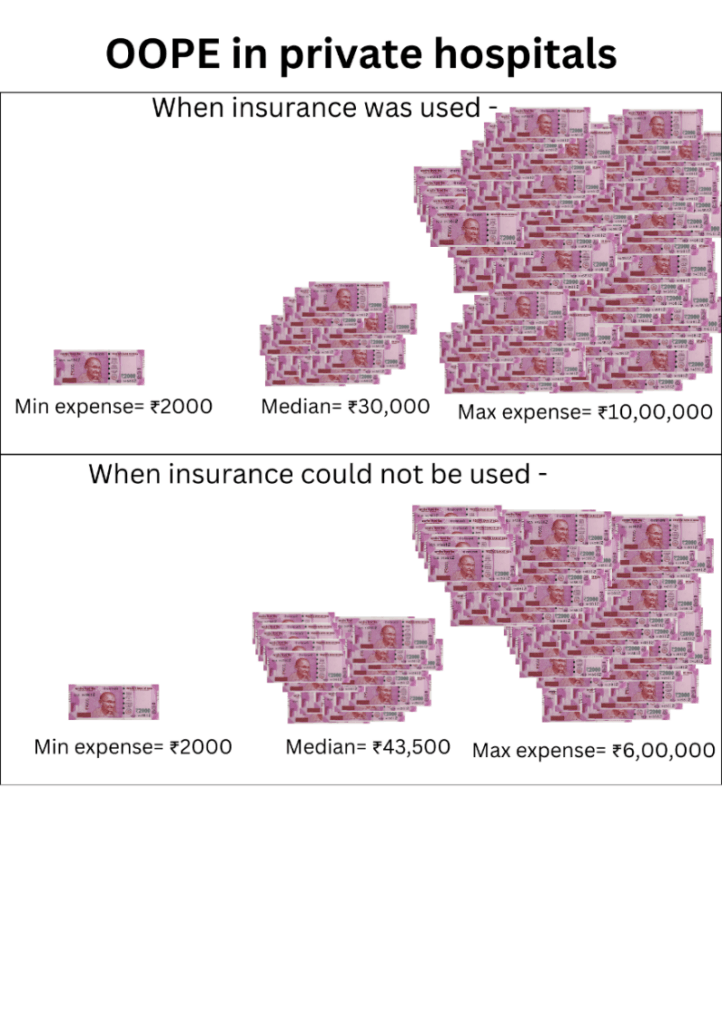
One can observe from the above charts that most people with a card or insurance would end up spending same or more than those who did not have a card. One thing is obvious that having a card or insurance is not going to make much difference in government/private hospitals.
Lessons From This Study
- Illnesses that need hospitalization are impoverishing the marginalised communities. The participants for this study were all from the working-class population, members of various trade unions, rural and tribal communities and thus were from the marginalised communities.
- It is evident that Out-of-Pocket (OOP) is a major economic burden on the marginalised communities.
- The much-touted insurance cards and insurance schemes are hardly making any impact and not serving the purpose of reducing OOP expenses and providing care for marginalised communities.
- Moreover, the processes involved in utilising insurance – like getting referral codes, approval, breach of privacy/ consent in taking patient’s pictures even in government hospitals are dehumanising and taxing for people who are already sick.
- In cases of emergencies, AB-ArK has a provision where patients can avail treatment in private hospitals and private hospitals to process the insurance. But in reality people are having to travel in sickness for approvals or end up spending high OOP.
- The numbers shown as success in terms of “coverage”, “beneficiaries treated”, “amount disbursed” are hiding these people’s lived realities.
- There seem to be several hurdles that have been created so that ultimately the needy can never get benefitted.
- Most secondary and tertiary care needs OPD care, multiple visits, and follow-up care. The current insurance models treat this care as episodic or one-off events and thus people are having to spend OOP.
Way Forward
- THE GOVERNMENT MUST STRENGTHEN GOVERNMENT HOSPITALS and SERVICES AND INCREASE THE BUDGET.
- We demand the government to stop insurance-based financing for healthcare but instead invest this in strengthening public institutions for Universal Healthcare.
- An SAA-K study has shown that prescription of medicines by government doctors to be purchased by patients from private pharmacies outside is rampant. This needs to be stopped totally through robust state supply of medicines and has already been done by Tamil Nadu, Kerala, and Rajasthan states.
- So also advising patients who have come to government hospitals for treatment being referred for various investigations outside at private laboratories is causing major economic drainage. The government facilities should have robust laboratory facilities.
- Empanelment of private hospitals by the government for delivering healthcare is not yielding any fruits and needs to be stopped. Instead, the government should use the money in strengthening the public health services.
- Stop all forms of Private Public Partnerships in delivering healthcare immediately. These insurances push people to rely on private health care and further lose trust in public institutions. Government’s responsibility is in building people’s trust through strengthening the public health system.